About Brain Injuries
TBI and ABI
Traumatic Brain Injury (TBI) arises from traumatic insults to the brain and head (vehicle collisions, falls, sports injuries, assaults, electrocution).
Acquired Brain Injury (ABI) includes TBI plus non-traumatic causes (stroke, aneurysm, arterial venous malformation, tumors, anoxic events, surgical mishaps, infections).
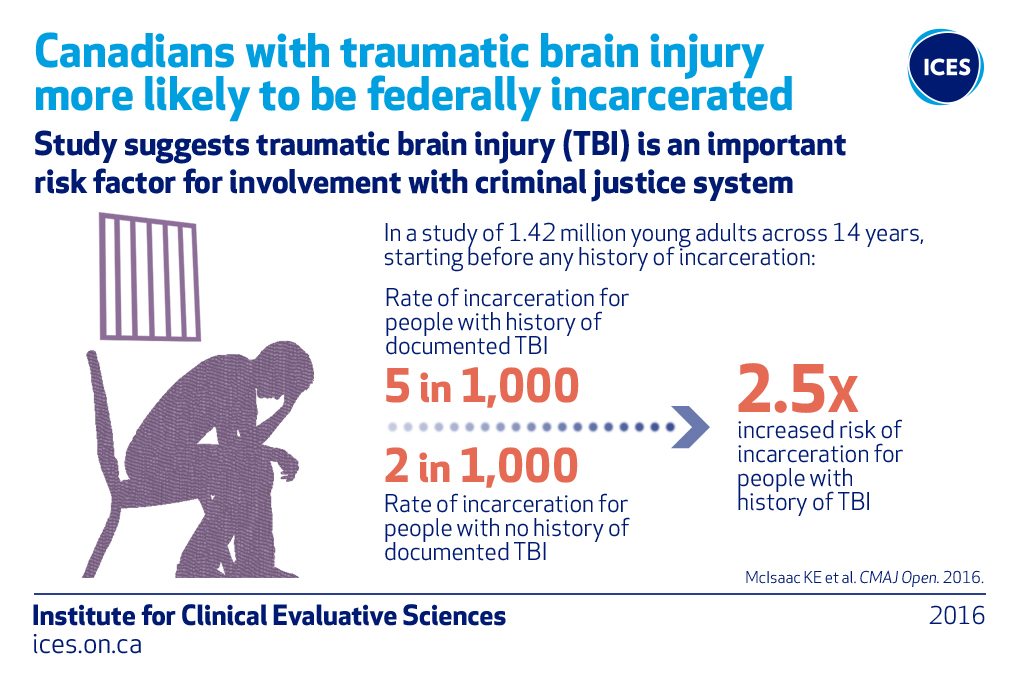
- TBI is estimated to occur at an annual rate of 5 per 1000 persons. (Langois JA, Rutland-Brown W, Thomas KE, Traumatic Brain Injury in the United States, Emergency Department Visits, Hospitalizations, and Deaths. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2006.)
- Statistically, TBI occurs at a rate 100 times that of spinal cord injury. (Won Hyung A. Ryu, Anthony Feinstein, Angela Colantonio, David L. Streiner, Deirdre R. Dawson, Early Identification and Incidence of Mild TBI in Ontario, The Canadian Journal of Neurological Sciences, Volume 36, Number 4, 429 – 435, July 2009.)
- When ABI and TBI are included together, estimates suggest up to 1 in 25 persons in Canada may be living with some level of ongoing disability from a brain injury.(Brain Disorders in Ontario: Prevalence, Incidence and Costs from Health Administrative Data, Ontario Brain Institute July 2015 at 148, incidence of TBI alone approaching 2% of population in Ontario in April 2010 assessment).
- While awareness and diagnosis of TBI is improving, missed cases, misdiagnosis and misattribution are commonly reported in the relevant clinic literature.(Silver, McAllister and Arcienegas, Textbook of Traumatic Brain Injury, 3rd ed. 2019; see also Zasler and Katz, Brain Injury Medicine: Principles and Practice, 2nd. Ed. 2012.)
- Post ABI, persons are seven times more likely to develop symptoms of mental illness.(Jeffrey M. Rogers; Christina A. Read; Psychiatric comorbidity following traumatic brain injury. Brain Injury, Volume 21, Issue 13 & 14 December, pages 1321 – 1333, 2007.)
“This funding allowed for the NBIA to provide case management services in over twenty-five (25) communities in northern BC.”
– Northern Brain Injury Association
The effect of brain injury is not limited to the health consequences for the victim.
- Youth convicted of a crime are more likely to have suffered a pre-crime brain injury.((Williams WH, Chitsabesan P, Fazel S, et al. Traumatic brain injury: a potential cause of violent crime? [published correction
appears in Lancet Psychiatry. 2018 Jul 17;:]. Lancet Psychiatry. 2018;5(10):836–844. doi:10.1016/S2215-0366(18)30062-2.)) - It has been estimated that over 85% of incarcerated individuals have a brain injury.((Slaughter B, Fann JR, Ehde D. Traumatic brain injury in a county jail population: prevalence, neuropsychological functioning
and psychiatric disorders. Brain Injury 2003;17(9):731-41.)) - A survey of Vancouver’s homeless population found that 66% reported a brain injury and of those 77% were injured prior to becoming homeless.((https://pacificaidsnetwork.org/files/2012/07/BC-Health-of-the-Homeless-Survey-FINAL1.pdf Krausz, Dr. Reinhard
Michael, British Columbia Health of the Homeless Survey Report, page 29, 2011.)) - Estimates put the brain injury rate among indigenous persons at 4-5 time the rate in the non-indigenous population.((Lasry O, Dudley RW, Fuhrer R, Torrie J, Carlin R, Marcoux J, Traumatic brain injury in a rural indigenous population in Canada:
a community-based approach to surveillance, doi: 10.9778/cmajo.20150105cmajo May 26, 2016 vol. 4 no. 2 E249-E259.))
“Brain Injury Alliance funding has enabled Fraser Valley Brain Injury Association to expand the number of programs offered to people with acquired brain injuries and their supporters. It has helped us to provide services in two more communities (Langley and Mission, BC) on a much broader scale than we were able to before with the addition of one staff person.”
– Fraser Valley Brain Injury Association
Why the alliance needs ongoing funding
Alliance funding helps British Columbians to get the assistance they need to move forward with their lives, putting them first in line to take advantage of an exciting future. Government’s support of the Brain Injury Alliance is a prime example of why British Columbia leads the nation in economic growth and social development.
- The Alliance has a strong 10 year track record in providing funding to community-led brain injury societies in BC.
- Alliance funding is vital to service provision for more than 4500 British Columbians with brain injury annually.
- The Alliance provides Government with cost-effective funds administration at less than 5% annually
- The Alliance funding has increased the stability of community brain injury organizations.
- The Alliance funding supports the growth of programs and services by leveraging of other grants, and fundraising dollars.
- The Alliance supports service providers:
- that focus on the unique needs of people who have survived an acquired brain injury
- provide vital services to individuals in an equitable way
- that provide a range of services to people with acquired brain injury
- that provide services that are not time-limited or based on third party payment
- Long term brain injury care is best understood and effectively managed at the community level.
- Community brain injury services provide second-stage recovery and facilitate the process of reintegration.
- The Alliance is committed to ensuring quality community services are available to those who need them, when and where they need them, in order to improve population health and assist government to achieve its goals.
